Media
HKUMed identifies an additional cost-effective drug option
for sedating patients with acute agitation in the emergency department
07 Mar 2022
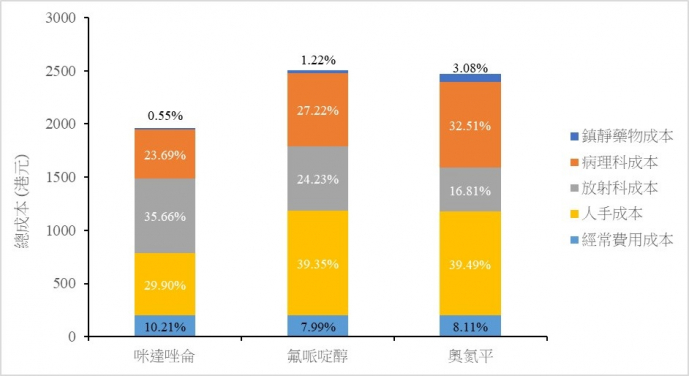
Cost components involved in the management of acute agitation in the A&E department for the base-case. All costs are in Hong Kong Dollars for the financial year 2019-2020.
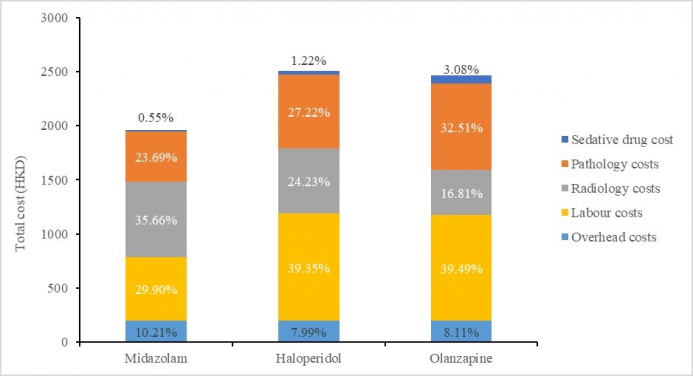
Cost components involved in the management of acute agitation in the A&E department for the base-case. All costs are in Hong Kong Dollars for the financial year 2019-2020.
- 1 / 2
- 2 / 2
Research led by the Department of Pharmacology and Pharmacy of the LKS Faculty of Medicine, The University of Hong Kong (HKUMed) has found intramuscular (IM) olanzapine to be another cost-effective drug for treating acute agitation in addition to traditional drug options used in Accident and Emergency departments (A&E) in Hong Kong. Compared with haloperidol, which is commonly used in A&Es, olanzapine is similarly cost-effective with a relatively more benign cardiovascular profile and causes fewer extrapyramidal side effects (movement disorders). The pharmacoeconomic findings are now published in Value In Health. [link to publication]
Background
Acute agitation is a common presentation at A&Es around the world. Prompt and effective care is important to reduce potential violence and harm to patients and those around them. Rapid sedation via the IM route is preferred in patients with acute agitation in emergency settings when the oral route of administration is not feasible. With the concerted efforts of the Department of Pharmacology and Pharmacy of HKUMed and clinical teams of six A&Es of the Hong Kong Hospital Authority (HA), a completed randomised clinical trial (RCT), published in EClinicalMedicine [link to the publication], found that IM olanzapine was safe and effective for sedating patients with acute agitation in A&Es. However, the higher unit drug cost of olanzapine could impact its application in clinical practice as a cost-effective treatment option compared to midazolam and haloperidol, two of the currently most commonly used IM sedatives in Hong Kong.
Research methodology and findings
The research team conducted a within-trial cost-effectiveness analysis comparing IM midazolam, olanzapine and haloperidol in the emergency setting, using data from a published multicentre RCT of six A&E departments in Hong Kong by the team.
The team found IM midazolam to be the more cost-effective drug option, while IM olanzapine and IM haloperidol were similarly cost-effective. IM olanzapine had a lower median cost (HKD 2,467.60 vs 2,504.60) but slightly lower effectiveness (116.70 vs 116.76 minutes of agitation-free time gained) compared to IM haloperidol. The incremental cost effectiveness ratio (ICER), defined as the additional cost of management in HKD per minute of agitation-free time gained, of IM olanzapine compared to IM haloperidol was HKD 727.69 per minute of agitation-free time gained. In patients with suspected underlying psychoses, the use of antipsychotics for rapid sedation is generally preferred in practice over benzodiazepines (such as midazolam) to prevent over-sedating the patient and preserve the opportunity for psychiatric follow up and assessment. In cases where the use of benzodiazepines is less desirable, IM olanzapine could be a preferred alternative over IM haloperidol since it has a more favourable adverse effect profile and is as cost-effective as IM haloperidol. The team also found that labour cost accounted for a significant portion of overall agitation management cost in the emergency setting (~30-40% in the base case, >70% when excluding investigational costs) whereas unit drug cost is relatively negligible (~0.5-3% in the base case, <10% when excluding investigational costs).
Research significance
Through this research, the HKUMed team was the first to provide the necessary evidence on the comparative cost-effectiveness of the three drug options for acute agitation management in A&Es. The findings serve to support formulary decisions on introducing and broadening the use of IM olanzapine for acute agitation in the emergency department. Subsequent to the RCT findings, IM olanzapine was incorporated into local A&E clinical guidelines by the Hospital Authority and added to the A&E drug formulary at the Hong Kong West Cluster. The latest pharmacoeconomic findings are expected to drive the expanded implementation/adoption of IM olanzapine at additional HA clusters.
‘We wish to thank the staff at Queen Mary Hospital and all the clusters who supported and participated in this multicentre, multidisciplinary research. This is a remarkable achievement for Accident and Emergency departments across Hong Kong,’ said Dr Esther Chan Wai-yin, Associate Professor of the Department of Pharmacology and Pharmacy and Research Lead of the Centre for Safe Medication Practice and Research (CSMPR), Department of Pharmacology and Pharmacy, HKUMed.
In addition, an increase in the trends of mental illness has been reported globally1, particularly during the COVID-19 pandemic. Findings from this study therefore underscore the importance of exploring and expanding safe, effective medication options for the management of behavioural emergencies in the A&Es, where new-onset mental illness, self-harm, drug and/or alcohol intoxication and mixed diagnoses are often present.
About the research team
The Hong Kong IM sedation research team is led by Dr Esther Chan Wai-yin, Associate Professor of the Department of Pharmacology and Pharmacy and Research Lead of the CSMPR, Department of Pharmacology and Pharmacy, HKUMed; Honorary Research Associate of the Department of Pharmacy, The University of Hong Kong-Shenzhen Hospital; Member of the Shenzhen Institute of Research and Innovation, The University of Hong Kong, Shenzhen; Associate Professor of the Laboratory of Data Discovery for Health (D²4H), Hong Kong SAR, China; and an affiliate in the Department of Accident and Emergency and the Department of Pharmacy, Queen Mary Hospital.
Mr Vincent Yan Ka-chun, a Hong Kong registered pharmacist and a PhD student of the CSMPR, Department of Pharmacology and Pharmacy, HKUMed, is the first author of the pharmacoeconomic publication. Ms Miriam Haendler, School of Pharmacy, University College London, United Kingdom; Dr Hayden Lau, Accident and Emergency Department, Queen Mary Hospital; Dr Shirley Li Xue, Assistant Professor of the Department of Medicine, School of Clinical Medicine, HKUMed; Dr Kim Lao Shijian, Global Medical and Scientific Affairs, Merck Sharp & Dohme, Hong Kong and a former PhD student of the CSMPR, Department of Pharmacology and Pharmacy, HKUMed; Dr Tsui Sik-hon, Accident and Emergency Department, Queen Mary Hospital and Honorary Clinical Professor, Department of Emergency Medicine, School of Clinical Medicine, HKUMed; Dr Celene YL Yap, Centre for Integrated Critical Care, The University of Melbourne, Australia; and Professor Martin RJ Knapp, Care Policy and Evaluation Centre, London School of Economics and Political Science, United Kingdom are the co-authors. Dr Esther Chan Wai-yin is the corresponding author of the pharmacoeconomic study.
Dr Esther Chan Wai-yin and Dr Kim Lao Shijian also contributed equally to the RCT and are co-first authors. Co-authors of the RCT include Ms Lam Lam, Clinical Research Associate, IQVIA, Hong Kong and former CSMPR research assistant; Dr Tsui Sik-hon, Accident and Emergency Department, Queen Mary Hospital and Honorary Clinical Professor, Department of Emergency Medicine, School of Clinical Medicine, HKUMed; Dr Lui Chun-tat, Accident and Emergency Department, Tuen Mun Hospital; Dr Wong Chi-pang, Accident and Emergency Department, Pamela Youde Nethersole Eastern Hospital; Dr Colin A Graham and Dr Cheng Chi-hung, Accident and Emergency Medicine Academic Unit, The Chinese University of Hong Kong and Department of Emergency Medicine, Prince of Wales Hospital; Dr Chung Tong-shun, Accident and Emergency Department, Ruttonjee Hospital; Dr Lam Hiu-fung and Dr Ting Soo-moi, Accident and Emergency Department, United Christian Hospital; Dr Jonathan C Knott, Department of Critical Care, University of Melbourne, Australia; Dr David M Taylor, Emergency Department, Austin Hospital, Australia and Department of Medicine, University of Melbourne; Dr David CM Kong, Pharmacy Department, Ballarat Health Services, Australia; Dr Leung Ling-pong, former Clinical Associate Professor, Department of Emergency Medicine, School of Clinical Medicine, HKUMed. Dr Esther Chan Wai-yin and Professor Ian Wong Chi-kei, Lo Shiu Kwan Kan Po Ling Professorship in Pharmacy, Head and Professor, Co-Director of CSMPR, Department of Pharmacology and Pharmacy, HKUMed; and Research Department of Practice and Policy, UCL School of Pharmacy, London, United Kingdom are the corresponding authors of the publication on the RCT. Professor Bernard Cheung Man-yung, Sun Chieh Yeh Heart Foundation Professor in Cardiovascular Therapeutics, Clinical Professor, Department of Medicine, School of Clinical Medicine, HKUMed; Professor Benjamin Cowling, Chair Professor of Epidemiology, Division Head of Epidemiology and Biostatistics, School of Public Health, HKUMed; Dr Ho Hiu-fai, Honorary Clinical Associate Professor, Department of Emergency Medicine, School of Clinical Medicine, HKUMed; and Dr Tse Man-li, Centre in-charge, Hong Kong Poison Information Centre, United Christian Hospital were members of the Data Safety and Monitoring Board.
Acknowledgements
This study was supported by the Research Grants Council, Government of the Hong Kong SAR, China (Ref No.: 789813).
Media enquiries
Please contact LKS Faculty of Medicine of The University of Hong Kong by email (medmedia@hku.hk).
1Mental Health, World Health Organization (https://www.who.int/health-topics/mental-health#tab=tab_2).
